my first week in tanzania was really interesting. obviously, you all read about my severe “homesickness” from kenya, which I should let you know I am almost over. I still miss the kids at little ray of hope like crazy, and I really miss my host sisters, but I don’t feel as upset about it as I was 11 days ago. but I am going back to nairobi for a weekend visit in my couple of weeks… I just spoke to anna and vicky and makena, and I miss them all so much, I will happily spend money on buying another visa to re-enter kenya, and then to re-enter tanzania. I might be crazy, in fact I know I am, but it’s only 250km away.
anyway, tanzania. I have been placed in a clinic called kijenge RC dispensary, RC stands for roman catholic. so there’s usually a few church songs playing in the background during the working hours, which definitely make me feel like I’m in a gospel choir or something (that’s my ultimate dream, to be a gospel singer. I’m just not a good singer nor am I black enough… one day). there’s two huge (and I don’t mean tall) nuns who run the show who I’m waiting for them to start singing “oh happy day”. the clinic is quite nice, they don’t need for much. I’ve had a look in their pharmacy and it’s stocked to the brim – they obviously have great sponsorship.
my first couple of days there were relatively observational, which I expected, and to be honest, it’s really captivating as people just don’t go to the doctor in australia for these sort of things. I sit in with the doctor (who is also my supervisor) as he does consults , and some really interesting cases have come through over the past week. the doctor is awesome, he includes me in the consults and asks my opinion, as well as translating to me what the patients say and what he thinks they have and what he will prescribe, and asks if patients in australia would receive the same treatment. I’m not completely up to date with what diagnoses require what medication, but a few things I recognised and could say yes or no. obviously we don’t have malaria cases back home.

the doctors office; the wall I sit and look at while he chats to the patients
things that came through the clinic last week include (but certainly not limited to):
– 3yo girl with malaria
– 25yo female with hypertension (220/150 on both arms)
– 6yo boy with mumps
– HIV positive woman for medication to prevent spread of disease to kid (niverapine)
– 25yo guy with cut finger
– 6yo boy with UTI
– 30yo female for stitches removal post caesarean
– 8 month old baby boy with otitis media
– 18yo girl with malaria
– 14yo girl with mumps
– baby with facial skin rash whose mother is HIV +
– 8yo boy and his 30yo dad with amoebiasis (a type of gastro) – treated with flagyl (metronidazole)
– 18 month old girl with bronchitis
– 5yo boy with productive chesty cough
– 3yo boy with malaria
– 5yo boy with huge abscess behind right ear (lidocaine before lancing, hardly done at all kid screamed the whole time, lots of shit (obviously not a medical term) came out)

hand washing facilities in the treatment room… yep, gross.
I spent one day working alongside a midwife doing antenatal checkups; learnt how to measure fundal height (basically measuring how big a women’s pregnant stomach is… that’s a very lay person description) and how to listen for a heartbeat with an archaic tool that looks like a weird mini-trumpet but not before harassing the baby through mum’s tum to figure out where the head is, therefore where the chest/heart might be (I’m still practising this new and difficult skill).

some of the things in the treatment room, apparently anything inside the silver tins is sterile. yet to see a steriliser though
some awesome things I learned this week:
– all malaria tests and treatment are free; children just don’t die of malaria here anymore as treatment is free (provided they can make it to a clinic)
– all tuberculosis tests are free
– all HIV testing and treatment are free
I still can’t wrap my head around the fact that we had three mumps cases in the clinic. for those of you who don’t know, mumps is one of the things that we’re all vaccinated against in the big MMR injection (measles, mumps and rubella) at 12 months of age and (I think) the booster is at 2 years. mumps is a viral infection that usually causes painful swelling of the salivary glands, but can cause other serious problems including encephalitis (swelling of the brain), which can lead to permanent brain damage and/or deafness.
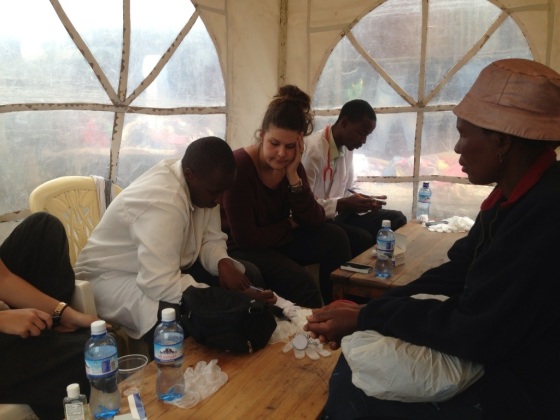
I was dumbfounded. like measles, isn’t mumps ‘extinct’? I mean obviously nothing is ever completely extinct – except dinosaurs- as these patients had it. even things like the bubonic plague (the black plague) have surfaced in madagascar and the middle east in the past few months. crazy stuff. I guess because I’ve not seen it in australia, and I know I certainly don’t have an extensive work history due to only just finishing uni, but I’ve never heard or seen anyone being diagnosed with mumps, at least not my age or younger. even though vaccines are pretty much readily available here in east africa (as far as I’ve seen), there are many factors that prevent kids being vaccinated against things that we’ve all been vaccinated against – unless you’re one of those crazy people who believes there’s a correlation between receiving certain vaccines and developing autism. don’t even get me started on that, that’s a topic for another day and a lot of wine… moving on… one website writes about the challenges of getting kids vaccinated here; i) lack of medical personnel to administer the vaccines, ii) lack of vaccines, iii) inability to store refrigerated vaccines in rural areas, iv) inability to transport refrigerated vaccines and v) poor record-keeping (reference: east africa partnership). I’ve seen all of these things, even to the point of only being able to have certain vaccines at the medical camps I worked at in kenya.

beautiful baby girl with the awful skin rash on her face, likely correlated to being HIV+
the baby girl who had the facial skin rash was such a beautiful little kid, I managed to take a picture (obviously after checking it was okay with her mum and the doctor). she wasn’t the patient, but the doctor and I obviously noticed something was wrong. her mum was coming in for more HIV anti-retrovirals (ARV’s) and the doctor mentioned that the baby’s skin rash is almost 100% indicative that she is also HIV+. I’ve done a lot of google-ing about rashes that relate to HIV and haven’t seen many that correlate to the same rash as the baby, but her mum didn’t consent to having her daughter tested on the day. the frustrating part of our job; you can’t force anybody, even when it’s in their or their child’s best interest.
it’s been really eye opening. and I’ve learnt a lot. not in terms of clinical skills, and by no means are they improving, but I’m learning a lot about patient care and how important it is for patients to feel like they’re being listened to. picking up on small cues about how certain medical professionals look at and/or speak to (or don’t) their patients; I know how much they drummed it into us at uni that you need to give patients eye contact so they aren’t feeling ignored. I thought it might have been a culture thing, but now I don’t, because patients are constantly looking at the doctor or midwife, hoping for some sort of interaction, yet they rarely receive it.
on a side note: I’m totally and utterly exhausted. I had no idea how tiring this volunteering thing would be, and I think I’ve been chronically tired since mid-september. dragging myself out of bed some days has been really difficult, I’m really sick of not showering (when the power goes off here in tanzania, so does the power, so you have to get water out of the well in our front yard to bathe with), I’m so so sick of eating carbs and carbs and more carbs (dinner the other night was spaghetti and mashed potato), I’m so tired of having irregular bowel movements and getting ‘travellers diarrhoea’ on a regular basis (yes that’s an overshare but I don’t give a shit) and spending every fortnight sick like I am now.
but it’s made worth it by a lot of little things – including an elderly gentleman who paid for my bus ride home from town yesterday to thank me for what I’m doing for his community. this guy was so unbelievably old (I always say that africans always look young, until they hit a certain age, then they look 150 years old), and had hardly any teeth left, and spoke terrible english, but I felt so humbled by how generous his gesture was. or by the kids and how they have to run their hands over your skin to admire how different the colours are… or pull your arm hairs out.
I’d be lying if I said I wasn’t counting down until my holiday in zanzibar, only 27 days until I’m lying on a beautiful, idyllic, crystal clear beach and actually relaxing. bring it on, baby. I’ll be so ready for a break by then!